 Climbing since 2000, the opioid epidemic has claimed more than 300,000 lives in the U.S. If the current trend continues, more than 650,000 people could die from opioid overdoses in the next 10 years. Some state and federal lawmakers are engaged in fighting the epidemic through a variety of methods—by educating providers and the public, increasing access to medication-assisted treatment (MAT) for opioid use disorders (OUD), increasing access to the opioid overdose reversal drug naloxone, and more. Yet, one of the key populations affected by the epidemic, people experiencing incarceration, has been substantially neglected by state and federal efforts.
Climbing since 2000, the opioid epidemic has claimed more than 300,000 lives in the U.S. If the current trend continues, more than 650,000 people could die from opioid overdoses in the next 10 years. Some state and federal lawmakers are engaged in fighting the epidemic through a variety of methods—by educating providers and the public, increasing access to medication-assisted treatment (MAT) for opioid use disorders (OUD), increasing access to the opioid overdose reversal drug naloxone, and more. Yet, one of the key populations affected by the epidemic, people experiencing incarceration, has been substantially neglected by state and federal efforts.
In the 1980s and 1990s, the federal and state governments addressed the crack cocaine epidemic through a war on drugs—they criminalized addiction by establishing mandatory minimums and incarcerating black people. Today, with an opioid epidemic that affects mostly white people (but has impacted many black people as well), the same governments are pouring money into prevention and treatment programs for people with opioid use disorders. Yet, black communities are still disproportionately impacted by drug-related incarceration as compared to white populations. Largely because the country continues to pursue a criminal justice and not a public health approach to OUD, particularly for black people, at least a quarter of the people in U.S. prisons have an OUD. States, however, are failing to provide incarcerated people with adequate treatment options for this medical condition and slow down the opioid epidemic.
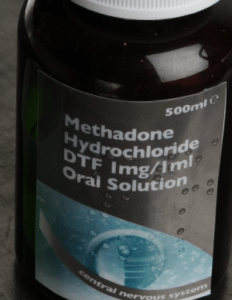
Most states are currently not providing the full range of MAT for inmates with OUD. Eight states do not provide any of the three FDA-approved medications for treating OUD to incarcerated individuals (methadone, buprenorphine, and naltrexone). Twenty-six states only offer naltrexone for re-entry, the medication with the least evidence behinds its effectiveness. Finally, in the 15 states that offer some combination of methadone, buprenorphine, and naltrexone to their inmates, the numbers overstate the level of access that inmates have to OUD medications, as an individual’s ability to obtain and fill a prescription varies between prisons. Since withdrawal symptoms can be painful and sometimes deadly, some courts have ruled that failure to provide appropriate treatment may constitute cruel and unusual punishment that violates inmates’ Eighth Amendment rights.
To date, Rhode Island is the only state that provides its inmates with all three FDA-approved medications to treat opioid addiction. The program appears to be working—a recent study found that it has cut overdose deaths among released inmates by almost 70 percent. These findings support the decades of research showing that MAT is the best path to recovery for people with an OUD.
MAT is also essential for individuals with OUD who have been recently released from prison. Without MAT, formerly incarcerated people rejoin their communities with reduced tolerance and a high susceptibility to a deadly overdose. A study published in the New England Journal of Medicine found that during the two weeks after their release, former inmates’ risk of a fatal drug overdose can be 129 times higher than for the general population.
This high risk of drug overdose touches on another issue—Medicaid coverage. Once released from prison, individuals with OUD continue to need access to treatment and other behavioral health services. However, despite clear federal guidance from the Centers for Medicare and Medicaid Services that Medicaid eligibility should not be terminated solely due to incarceration, Medicaid recipients often lose coverage while in prison and may experience challenges regaining coverage after their release. State policies on reestablishing Medicaid coverage for formerly incarcerated people vary greatly from state to state. As of July 2016, 16 states suspend Medicaid coverage only for the duration of an individual’s incarceration, allowing quick and seamless reactivation of coverage upon release. Another 15 states suspend Medicaid only for a specific period of time. This may allow people who are incarcerated for short periods to quickly reactivate their coverage but forces those incarcerated for longer periods to have to reapply. Nineteen states illegally terminate Medicaid coverage altogether when an individual is incarcerated, forcing them to fully reapply upon release.
If states fail to fully reinstating Medicaid coverage upon release, they are preventing individuals with OUD from obtaining their only method to access treatment. All state Medicaid programs cover at least one MAT medication, and most cover all three. Since the two weeks after release present the highest risk of overdose for formerly incarcerated people, it is a crucial time period in which access to MAT may be the most determinative factor in whether a person lives or dies.
By failing to address the treatment needs of people experiencing incarceration, states are allowing a crucial opportunity to quell the opioid epidemic to slip from their hands. All states should pass legislation or change regulations and policies to eliminate the gap in Medicaid coverage after a person is released in prison. They should also follow Rhode Island’s lead in offering FDA-approved medications—particularly methadone and buprenorphine—for treating OUD in prisons. These methods alone will not stop the opioid epidemic, but they can help prevent overdose deaths, making them worthwhile investments in our nation’s public health.

