The Eligibility & Enrollment team at the National Health Law Program (NHeLP) works to ensure that low-income people can access the health coverage and care they need in two ways: first, by expanding who is eligible for affordable, quality health coverage, and second, by ensuring that paperwork and state Medicaid systems do not prevent eligible people from enrolling and staying covered.
While the Affordable Care Act (ACA) substantially expanded Medicaid eligibility, there are still gaps in who is able to get coverage. Not all states have adopted Medicaid expansion and the ACA did not remove long-standing restrictions on immigrants’ eligibility for Medicaid. Meanwhile, overly complicated application and renewal processes mean that many eligible people lose Medicaid coverage for “procedural” reasons, like failing to return a form even though it had been mailed to the wrong address.
We engage with state-level advocates and the US Department of Health & Human Services through its Centers for Medicare & Medicaid Services (CMS) to improve eligibility pathways, simplify enrollment policies and practices, and streamline renewal processes so that more people are eligible for and enrolled in vital health coverage. NHeLP’s Eligibility & Enrollment team also educates advocates across the country on eligibility and enrollment rules and best practices, and develops materials and publications to support advocates assisting low-income health care enrollees on the ground. We endeavor to apply an equity lens to all of our work, and we are vigilant in our efforts to ensure that Black, Indigenous, and people of color, immigrants, individuals with limited English proficiency, and people with disabilities can enroll in—and retain—coverage in a person-centered, equitable way.
During the Medicaid unwinding, NHeLP’s Eligibility & Enrollment team provided critical support to state-level advocates as state Medicaid agencies embarked on the largest undertaking of Medicaid renewals in the program’s history. Although the official unwinding has ended, eligibility and enrollment issues persist, and NHeLP’s team will continue to work to address these issues.
Eligibility & Enrollment Priorities and Resources
Our Eligibility & Enrollment team works with staff across the National Health Law Program to advance more expansive and accessible Medicaid enrollment and retention. The team priorities are Eliminating Administrative and Procedural Barriers, Disability Access, Language Access, and Immigrant Health. Follow the links below to learn more.
Intersection of Federal Policy and Eligibility & Enrollment
Our Eligibility & Enrollment team works to expand who is eligible for Medicaid coverage and make it easier for eligible people to stay enrolled without unnecessary barriers. On a federal level, this includes administrative advocacy to improve eligibility policies, simplify application processes, and streamline renewal practices; coalition work to bring local, state, and identity-based partner groups to the policy table; and educational efforts to keep advocates and policymakers informed about the best practices to promote sustained, comprehensive Medicaid coverage. By advocating for more straightforward and accessible policies and practices, we aim to make sure that everyone who needs Medicaid is able to get and keep coverage, free from discriminatory and inaccessible barriers.
In addition to federal advocacy, NHeLP also works on policy in California. For more information about our California policy work, please visit our California Eligibility & Enrollment page.
Learn more about Eligibility & Enrollment Litigation at NHeLP
All too often, Medicaid enrollees’ coverage is threatened without the required processes that protect their access to critical health care. NHeLP litigates to ensure that states comply with federal non-discrimination and eligibility and enrollment laws when making Medicaid decisions. We also work to guarantee that applicants and enrollees receive clear notices explaining these decisions and have access to a fair hearing to contest them.
For decades, NHeLP has used litigation and administrative complaints to bring about meaningful changes in eligibility and enrollment practices for the millions of people insured by Medicaid. Our Litigation & Enforcement team also works alongside our Health Law Partners to protect coverage on a state-level. Learn more about our Eligibility & Enrollment cases by expanding the link below, and find out more about all of our cases on the Litigation & Enforcement page.
Eligibility & Enrollment Blogs
Eligibility & Enrollment News
NHeLP’s Eligibility & Enrollment team collaborates with our Communications team to effectively message and promote eligibility and enrollment-related policies and issues to the media, ensuring broader awareness and support for these critical matters. Journalists looking to connect with our Eligibility & Enrollment team should contact communications@healthlaw.org.
Meet the Eligibility & Enrollment Team

Elizabeth Edwards
Senior Attorney
Elizabeth Edwards is a Senior Attorney in the National Health Law Program’s North Carolina offices. In addition to working…

Alicia Emanuel
Senior Attorney
Area(s) of Expertise: California, Medi-Cal Eligibility, Covered California, Exchange Coverage, Children's Health, CA Children's Services Program Alicia Emanuel is…

Sarah Grusin
Senior Attorney
Area(s) of Expertise: Due Process, Immigrant Access to Care, Algorithms and Computer Systems, 1115 Waivers, Court Access and Private…

Miriam Delaney Heard
Senior Attorney
Miriam Delaney Heard is a Senior Attorney in the National Health Law Program’s North Carolina office. In addition to…

Shandra Hartly
Staff Attorney
Shandra Hartly is NHeLP's Staff Attorney. She works with Eligibility and Enrollment, and the Services practice areas. Before joining…

Kimberly Lewis
Managing Director, California Advocacy and Practice Area Managing Director
Kimberly Lewis is the Managing Director, California Advocacy and Practice Area Managing Director at the National Health Law Program’s…
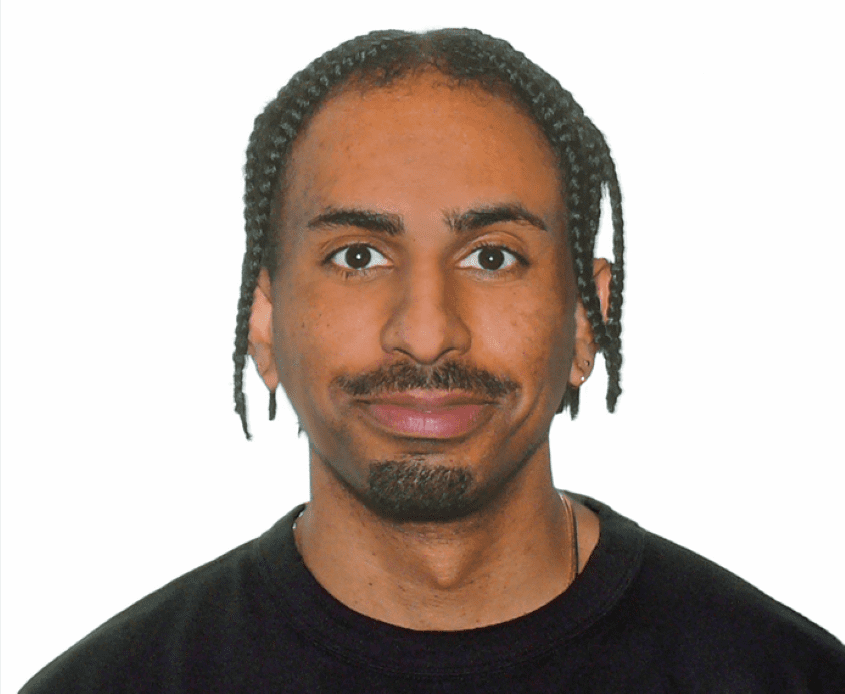
Jules Lutaba
Senior Attorney
Jules Lutaba is a Senior Attorney at the National Health Law Program, based in California. His work involves a…

Skyler Rosellini
Assistant Director of California Policy
Skyler Rosellini (he/him) is the Assistant Director of California Policy at the National Health Law Program in Los Angeles,…

Mara Youdelman
Managing Director, Federal Advocacy
Areas of Expertise: legislative and administrative advocacy, nondiscrimination protections (including Section 1557 of the ACA & Title VI of…




